- | Healthcare Healthcare
- | State Testimonies State Testimonies
- |
South Carolina's Certificate-of-Need Program: Lessons from Research
Testimony before the South Carolina Senate, Medical Affairs Committee, Certificate-of-Need Subcommittee
Chair Davis and distinguished members of the subcommittee:
My name is Matthew Mitchell. I am an economist at the Mercatus Center at George Mason University. In recent years, my colleagues and I have been studying certificate-of-need (CON) laws in healthcare. I am grateful for the opportunity to discuss our findings with you today.
Today, I will
- offer a brief history of CON laws,
- compare South Carolina’s CON program to the programs in other states, and
- give an overview of the economic evidence that has led many to conclude that these laws harm patients and taxpayers.
Introduction to CON Laws
CON laws require healthcare providers wishing to open or expand a healthcare facility to first prove to a regulatory body that their community needs the services the facility would provide. The regulations are typically not designed to assess a provider’s qualifications or safety record. Other regulations such as occupational licensing aim to do that. Instead, CON laws aim to determine whether or not a service is economically viable and valuable.
The process for obtaining a CON can take years and can cost tens or even hundreds of thousands of dollars in preparation costs. Although these regulations appear to benefit incumbent providers by limiting their competition, their effects on patients and taxpayers have generally been found to be negative. This finding helps explain why antitrust authorities at the Federal Trade Commission (FTC) and at the US Department of Justice (DOJ) have long taken the position that these rules are anticompetitive. In a joint report from 2004, for example, the FTC and DOJ declared,
The Agencies believe that, on balance, CON programs are not successful in containing health care costs, and that they pose serious anticompetitive risks that usually outweigh their purported economic benefits.
A Brief History of CON Regulation
More than four decades ago, Congress passed and President Ford signed the National Health Planning and Resources Development Act of 1974. The statute enabled the federal government to withhold federal funds from states that failed to adopt CON regulations in healthcare.
New York had already enacted the first CON program in 1964; by the early 1980s, with the federal government’s encouragement, every state except Louisiana had implemented some version of a CON program. Policymakers hoped that these programs would restrain healthcare costs, increase healthcare quality, and improve access to care for poor and underserved communities.
In 1986—after Medicare changed its reimbursement practices and as evidence mounted that CON laws were failing to achieve their stated goals—Congress repealed the federal statute, eliminating federal incentives for states to maintain their CON programs. Since then, 15 states, representing about 40 percent of the US population, have done away with their CON regulations, and many have narrowed their scope. A majority of states still maintain CON programs, however, and vestiges of the National Health Planning and Resources Development Act can be seen in the justifications that state legislatures offer in support of these regulations.
CON Regulation in South Carolina
South Carolina operates an extensive CON program, requiring providers to obtain permission before making changes to equipment, services, facilities, hospital beds, and nonhospital beds.
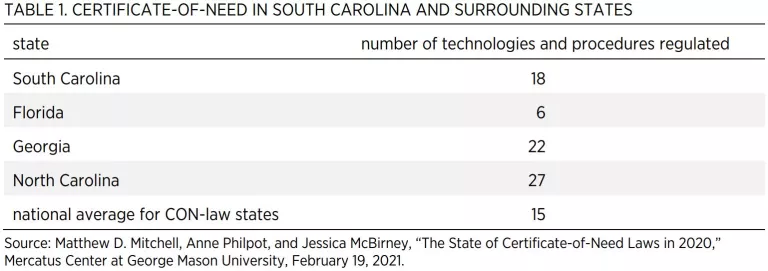
Table 1 shows the number of technologies and procedures regulated by South Carolina and by the surrounding states. Among all states with CON regulations, the average number of technologies and procedures regulated is 15. South Carolina regulates 18 technologies and procedures.
- Ambulatory surgical centers (ASCs)
- Cardiac catheterization
- Gamma knives
- Home health
- Hospice
- Hospital beds
- Intermediate care facilities (ICFs) for individuals with intellectual disabilities
- Linear accelerator radiology
- Long-term acute care (LTAC)
- Neonatal intensive care
- New hospitals or hospital-sized investments
- Nursing home beds/long-term care beds
- Obstetrics services
- Open-heart surgery
- Psychiatric services
- Radiation therapy
- Rehabilitation
- Substance/drug abuse
In addition, the state requires a CON whenever a facility adds any new service or expands a service at a cost of $2 million or more.
The Economics of CON Regulation
Unfortunately, by limiting supply and undermining competition, CON programs may undercut each of the laudable aims that policymakers desire to achieve with these rules. In fact, research shows that CON laws fail to achieve the goals most often given when enacting such laws. These goals include
- ensuring an adequate supply of healthcare resources,
- ensuring access to healthcare for rural communities,
- promoting high-quality healthcare,
- ensuring charity care for those unable to pay or for otherwise underserved communities,
- encouraging appropriate levels of hospital substitutes and healthcare alternatives, and
- restraining the cost of healthcare services.
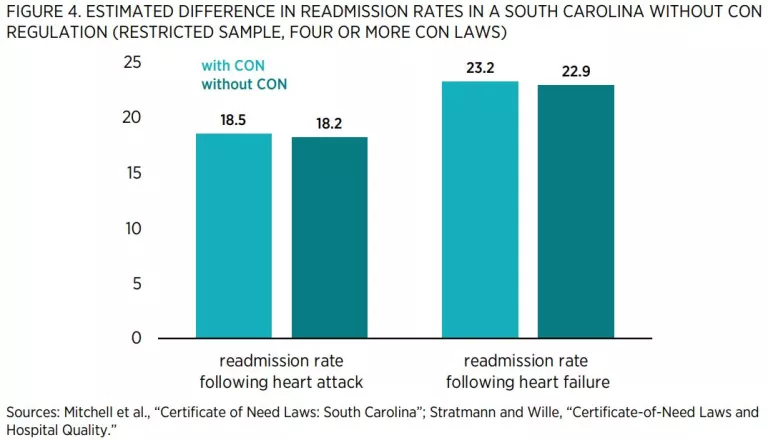
Researchers have ample information to help predict what would happen if South Carolina were to repeal its CON regulations because 15 states have repealed their CON programs, and others have pared theirs back. Economists have used modern statistical methods to compare outcomes in CON and non-CON states to estimate the effects of these regulations. These methods control for factors such as socioeconomic conditions that might confound the estimates. Table 1 summarizes some of this research. It is organized around the stated goals of CON laws.
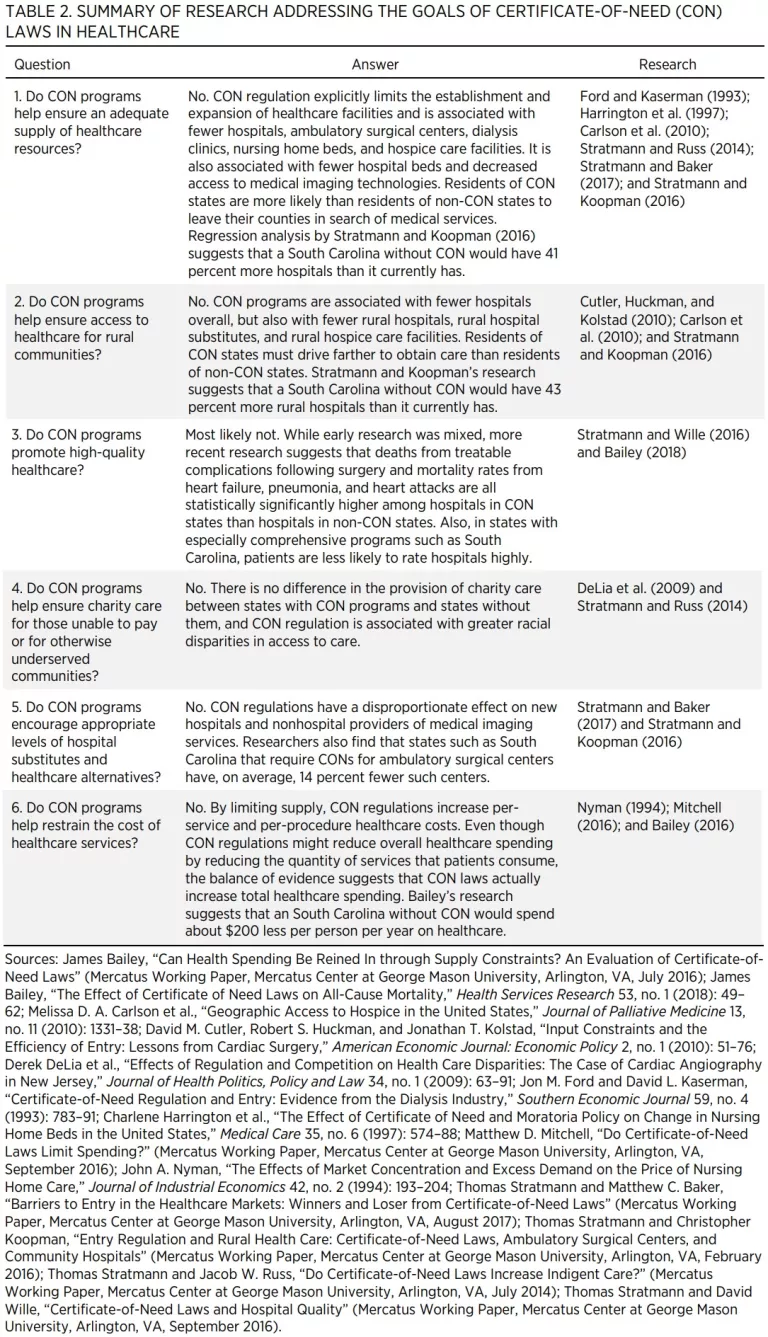
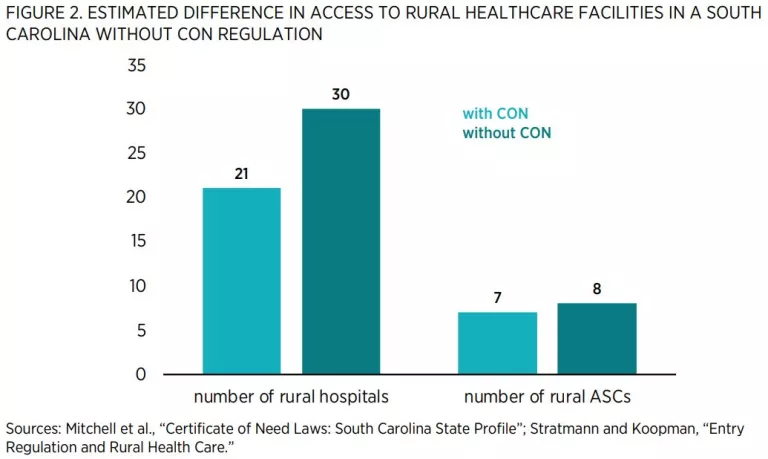
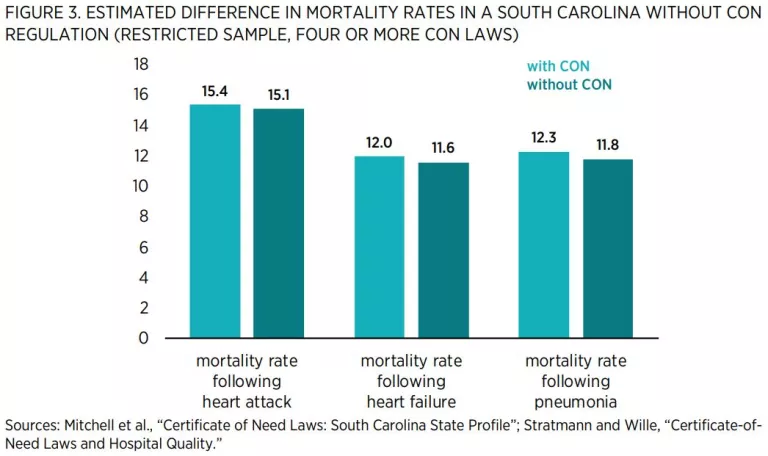
Figure 1 shows the actual number of hospitals and ASCs as well as the estimated number of hospitals and ASCs in an South Carolina without CON regulation.

Concluding Remarks
The weight of evidence suggests that a full repeal of CON laws would expand access to healthcare in South Carolina that is of both high quality and low cost. Repeal could be scheduled to take effect in the near future or at a later date. Alternatively, policymakers could phase in repeal by requiring the CON board to approve an ever-larger percentage of applications over a certain number of years.
Given the substantial evidence that CON laws do not achieve their stated goals, one may wonder why these laws continue to exist in so much of the country. The explanation seems to lie in the special-interest theory of regulation. Specifically, CON laws perform a valuable function for incumbent providers of healthcare services by limiting their exposure to new competition. Indeed, recent evidence suggests that special interest groups are able to use political donations to increase the odds that their CON requests will be granted. This aspect of CON regulation is one reason why economists as well as antitrust authorities have long believed that these regulations are anticompetitive and harmful to consumers.
For those who are interested in further details on the effects of CON laws on spending patterns, I have attached my paper, “Do Certificate-of-Need Laws Limit Spending?” Like all Mercatus Center research, it has been through a rigorous, double-blind peer review process.
Thank you again for the opportunity to share my research with you. I look forward to answering any questions you may have.
Attachment
“Do Certificate-of-Need Laws Limit Spending” (Mercatus Working Paper)

